ConsumerConnect High Touch
Prioritized outreach. Optimal health and costs.
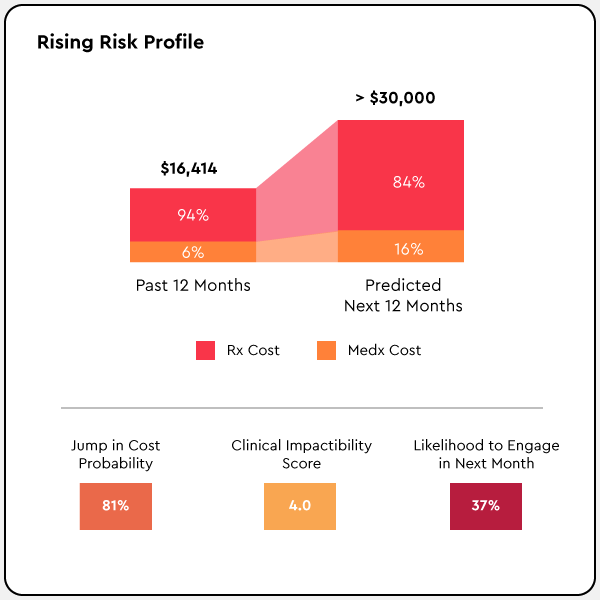
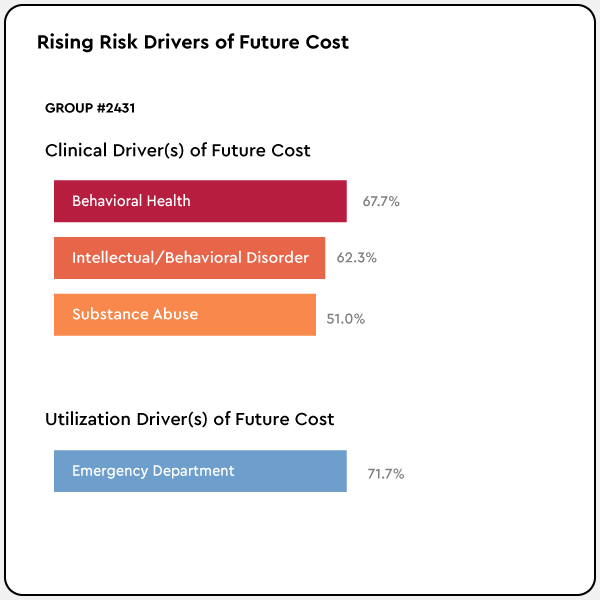
Prealize’s AI-powered platform generates proactive, personalized insights into future high-cost claimants that enable you to prioritize outreach based on cost drivers, clinical impact, and likelihood of member engagement. That lets you efficiently target your efforts, improve member health, and reduce costs.
Who needs ConsumerConnect High Touch
For clinical, health services, care management, and physician leaders
- Gain insight into future high-cost claimants and their cost drivers
- Achieve optimal member outreach efficacy and efficiency
- Improve member use of health programs and adoption of interventions
- Reduce avoidable costs through proactive care management and provider services
- Prioritize the allocation of scarce resources
Why you need ConsumerConnect High Touch
Our AI-powered proactive insight allows you to improve member health outcomes and reduce avoidable cost through high-touch care management.
Maximize scarce resources
Prioritize most in need outreach to maximize scarce care resources.
Predict up to 12 months sooner
Identify members at risk for a health condition up to 12 months before the diagnosis appears on the claim, so that you prevent issues that lead to high-cost claims.
Receive actionable, accurate insights
Receive curated member target lists based on member-level insight into rising risk, cost, drivers, likelihood to engage, and clinical impactability.
Streamline care management and physician workflows
Make it easy for staff and physicians through seamless integrations.
Results
Better
ROI
4:1
Get more for your money with a proven return
More
Lead Time
12+
Gain 12 months lead time to impact the health trajectory
Higher
Engagement
20%
Significantly increase telephonic engagement
How ConsumerConnect High Touch works
Our clinically-informed AI identifies priority member outreach based on cost drivers, clinical impact, and likelihood of member engagement.
- Member-level condition predictions enable you to intervene 12 months before a diagnosis hits the claim
- Gain additional lead time to impact the health trajectory
- Benefit from seamless workflow integrations and easy-to-understand visualizations of member trends
What our customers say
"You gave me my life back."
Maggie S, Health Plan Member
"Prealize gave me the right members at the perfect moment of impactability."
Shauna W, Care Manager, Large Health Plan
2022 State of Health: The Domino Effect
Nearly two years since COVID-19 first erupted in the United States, the true magnitude of its influence on the health of Americans is becoming much clearer—and much more troubling. The devastating and deadly virus has unleashed a domino effect of crises that, if left unmanaged, will continue to erode population health and increase healthcare spending for years to come.
Download