ConsumerConnect High Tech
The right members. The right outreach. The right outcomes.
Improve member experience and engagement by identifying the conditions members are most at future risk for—and connecting them to the right resource at the right time.
Who needs ConsumerConnect High Tech
For CX, member experience, and digital health leaders
- Supercharge the member healthcare experience and engagement with personalized, timely insights
- Influence the next-best action with predictive targeting with enough lead time to improve member trust and drive action
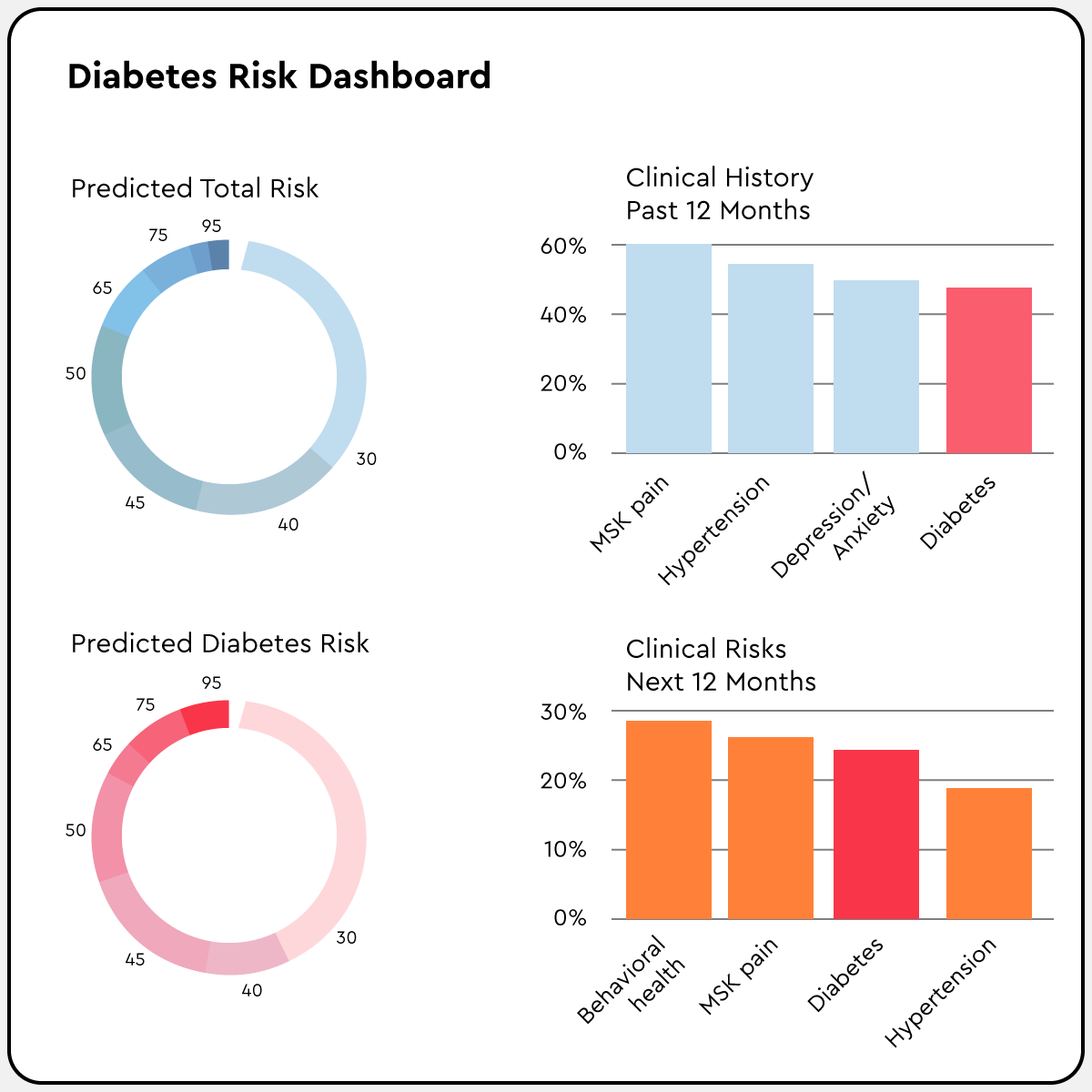
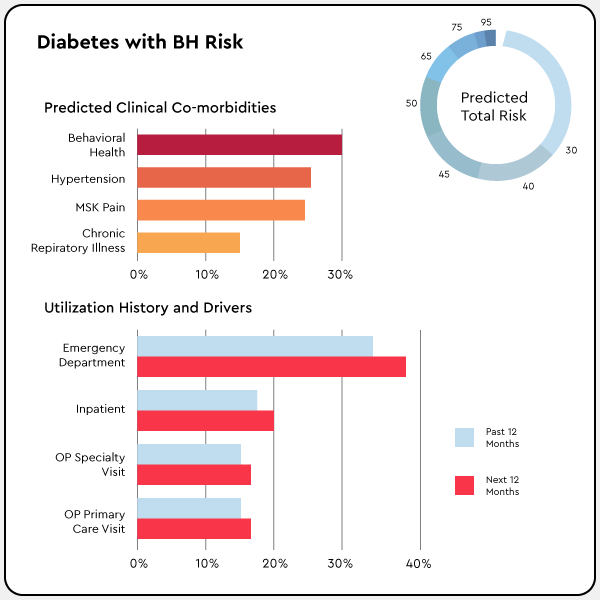
- Improve health outcomes and optimize investment in programs like behavioral health, diabetes, MSK, and ED diversion
- Deliver more value to members and customers
Why you need ConsumerConnect High Tech
In a world where shopping, banking, and travel are personalized to meet our needs and preferences, healthcare must rise to the challenge. Our targeted, personalized member-level insights drive a better healthcare experience and improve engagement. That means healthier members who are happier with their healthcare.
Access the "hidden" cohort
Use predictive intelligence and improve member targeting and steerage.
Gain personalized insights
Identify high-risk members 12 months before a diagnosis hits the claim, giving you time to build member trust and drive to high-value actions.
Improve program engagement
Supercharge member engagement with more accurate insights that enable personalized member targeting.
Results
More
Proactive
12+
Provided predictions 12 months before diagnoses hit claims so that the plan could act earlier
Identify
More
10%
Increase in identification of future risk over ED/IP utilization rules-based approaches
Better
Engagement
60%
Lift in behavioral health digital campaign engagement
How ConsumerConnect works
We match members to 35+ program categories, including high-cost, high-need areas like behavioral health, diabetes, and ED prevention—up to 12 months before diagnosis. Then, our platform integrates seamlessly with your existing platforms to power and prioritize targeted high-tech and high-touch interventions.
- Personalized member-level insights can be leveraged for all digital outreach, including vendor programs
- Earlier identification of conditions, with time to impact the healthcare experience
- Program engagement lists are based on member-level predicted conditions and procedures, future risk, and likelihood to engage
What our customers say
"You gave me my life back."
Maggie S, Health Plan Member
"This is cutting edge."
SVP, Underwriting, Large Blues Plan
"Prealize gave me the right members at the perfect moment of impactability."
Shauna W, Care Manager, Large Health Plan
2022 State of Health: The Domino Effect
Nearly two years since COVID-19 first erupted in the United States, the true magnitude of its influence on the health of Americans is becoming much clearer—and much more troubling. The devastating and deadly virus has unleashed a domino effect of crises that, if left unmanaged, will continue to erode population health and increase healthcare spending for years to come.
Download